From the Los Angeles Times 11/13/11 article, Red tape hampers care for patients who are poor and disabled.
Such patients qualify for Medicare and Medicaid, but bouncing back and forth between state and federal agencies can increase medical costs and reduce their quality of care.
M.C. Kim had four heart attacks in as many years. Each time, he left the hospital not knowing why his heart had failed. When he tried to enter a cardiac rehabilitation program to learn how to reduce the odds of having more heart trouble, the Medicare office told him to call Medicaid. The Medicaid office told him to call Medicare. In the end, he said, both denied coverage.
“I was like a pingpong ball,” said Kim, 51, who lives in Los Angeles. “Nobody wanted to take responsibility.”
So Kim kept returning to the emergency room, racking up expensive medical bills for taxpayers.
Kim and other patients like him are among the nation’s sickest and poorest residents, and their high-cost medical care places an untenable financial burden on states and the federal government. Because he is poor and disabled, he qualifies for both the federal Medicare program and the state-federal Medicaid program, called Medi-Cal in California.
These patients — 1.1 million in California alone — are some of the country’s priciest government healthcare consumers. Called dual eligibles, they accounted for close to 40% of Medicaid spending in California in 2009, nearly $10 billion, but constitute only about 15% of enrollees. Nationwide, the nearly nine million dual eligibles have similarly disproportionate outlays and cost roughly $250 billion annually in Medicare and Medicaid funds.
Now, as federal officials look for ways to control costs under healthcare reform, they are zeroing in on millions of patients like Kim. But system reform is a sensitive issue.
“It’s a much more fragile population,” said Casey Young, who works for AARP in California. “It is always concerning when the motivation is cost savings and not improving care.”
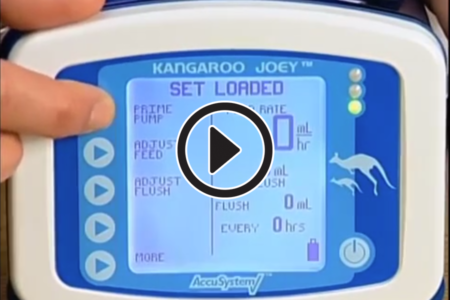
The government spends so much on dual eligibles because of their illnesses: multiple sclerosis, cerebral palsy, Alzheimer’s disease and other debilitating conditions. The expenditures also are high because patients bounce between the two plans and often receive unnecessary, duplicative and poorly coordinated services. They cycle through emergency rooms, hospitals and nursing homes more than other Medicare or Medicaid enrollees, according to the Kaiser Family Foundation.
The result, healthcare officials and other experts say, is not only inflated expenditures but also gaps in medical treatment for the most vulnerable patients: the elderly, poor and disabled.
“When beneficiaries have to navigate two programs separately, it is no surprise that the care they receive is often inefficient and ineffective,” Health and Human Services Secretary Kathleen Sebelius said in a speech in Washington, D.C., in September. “We can dramatically improve health outcomes and reduce costs for dual eligibles if we do a better job coordinating their care.”
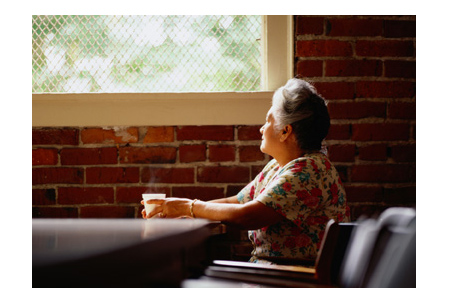
Bertha Poole, who is covered by both Medicare and Medicaid, said her problems navigating both programs have been small but extremely frustrating. Poole, a quadriplegic, lives on her own in an apartment equipped with special chairs and lifts. She relies on an aide to help her bathe, eat and dress.
When a wheel fell off her shower chair, it took nearly a year for her to convince Medi-Cal, California’s version of Medicaid, to fix it. “It sounds frivolous until you need it,” she said.
Dual eligibles typically qualify for Medicaid because they are poor and for Medicare because they are either elderly or disabled. Medicare pays for most doctor visits and hospital stays. Medicaid pays for what isn’t covered under Medicare, including long-term care at nursing homes.
Each program has tried to shift costs to the other. A federal study last year found that leads to higher bills for taxpayers, as well as lower-quality patient care. Among the problems driving up spending, the study said, are unneeded hospitalizations.
One often-cited example of the financial tug of war involves nursing homes. If a dual eligible in a nursing home gets pneumonia and is treated there, for example, Medicaid picks up the bill. But if the person is transferred to a hospital, Medicaid doesn’t have to pay. Medicare does.
“Patients get shuttled from one bed to the next and sometimes fall on the floor in between,” said Joe Baker, president of the Medicare Rights Center.
Kim, the heart patient, said better coordination might have prevented him from going to the emergency room roughly 20 times in the last six years.
“I appreciate the programs, but they are in such disarray,” he said. “There is so much red tape.”
The federal health reform law created new offices to coordinate care between Medicaid and Medicare and help states identify ways to curb costs. Earlier this year, California and 14 other states were awarded $1 million in federal grants to test ways to make those improvements.
In a trial effort set to begin in 2013, California plans to begin shifting several hundred thousand dual eligibles into managed care plans to serve all their healthcare needs.
Currently, the vast majority of the state’s dual eligibles are in health plans in which doctors and hospitals bill patients on the basis of services provided, meaning costs often soar quickly, healthcare experts say.
Managed care plans would reduce spending, state officials say, and make it easier for patients with complex health needs to get required care without receiving duplicate treatments or unnecessarily landing in nursing homes or hospitals.
“What we are trying to say is, ‘You don’t have to do this alone,’ ” said Jane Ogle, a deputy director in the state’s Department of Health Care Services. “And when we help you manage this, there are naturally going to be some savings.”
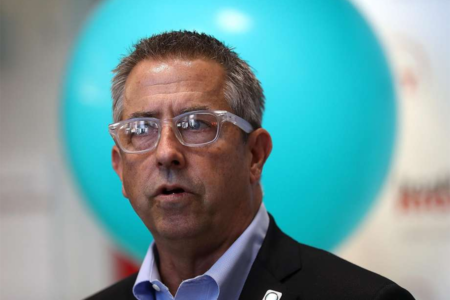
L.A. Care, the nation’s largest public not-for-profit health plan, has proposed taking on some of those patients in Los Angeles County. “It’s overdue to find a system of coordinated care for these folks,” said Howard Kahn, the plan’s chief executive. “We have got to get the costs of these public programs under some level of control.”
Dual eligibles and advocates for seniors and the disabled have mixed views about managed care’s ability to make things better. Some say having one place to go for medical care would be a huge improvement. Others worry that it could become harder to choose doctors.
Shelly Jerald, whose 27-year-old son Andre is developmentally disabled and enrolled in Medicare and Medicaid, said she has to handle all of his doctor appointments and bills. Recently, she had to make repeated calls to ensure that a bill from an eye doctor was paid by the right program. “If we could just talk to one person, that would make it easier for us lay people,” she said. “It’s so frustrating.”
But Carla Cleveland, 49, a dual eligible who has diabetes, arthritis, chronic pain and a history of pituitary tumors, fears that she will lose access to her doctors under managed care. Cleveland said she already struggles to get high-quality doctors to accept Medicare and Medicaid patients.
“I am just fearful about what is going to come,” she said.
Author: Anna Gorman